Throat Cancer Explained: Symptoms, Causes, Treatment & HPV Link | OncologyInsightsHu
Throat Cancer: The Complete Guide for Patients
Understanding Pharyngeal & Laryngeal Cancers: From HPV Link to Modern Treatments. Expert-Curated, Patient-Focused Insights.
🩺 Key Fact Summary
Prevalence: Accounts for ~4% of all cancers in the U.S. Major Shift: HPV is now a leading cause of oropharyngeal cancer. Prognosis Divergence: HPV+ cancers have significantly higher survival rates. Early Sign: Persistent hoarseness for >3 weeks demands an ENT evaluation.
What Exactly is "Throat Cancer"?
"Throat cancer" is an umbrella term for malignancies developing in the pharynx (throat) or the larynx (voice box). These are anatomically and functionally distinct from cancers of the mouth, esophagus, or trachea. Precise localization is critical for treatment planning.
Anatomy: The Two Key Battlefields
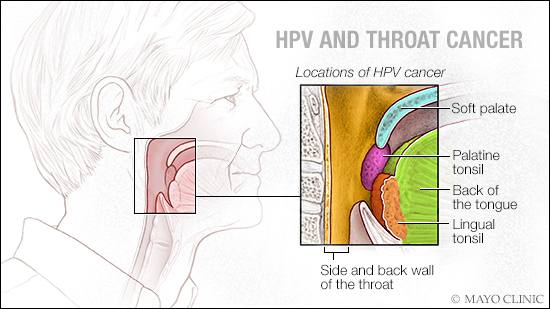
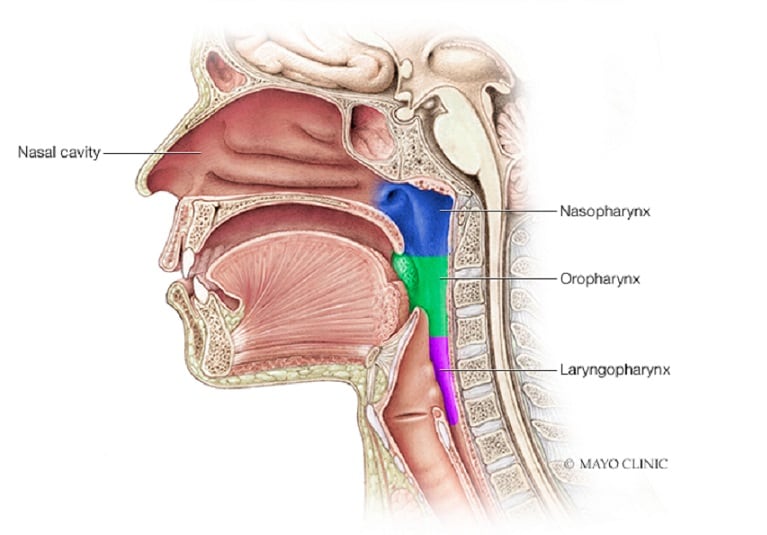
Labeled anatomy of the pharynx and larynx – key sites for throat cancers (NCI Visuals)
1. The Pharynx (Throat Proper)
A 5-inch muscular tube from behind the nose to the esophagus.
- 1 Nasopharynx: Behind the nose. Associated with Epstein-Barr Virus.
- 2 Oropharynx: Includes tonsils, base of tongue, soft palate. Primary site of HPV-related cancer.
- 3 Hypopharynx: Sides and back of the throat, surrounding the larynx.
2. The Larynx (Voice Box)
Houses the vocal cords. Divided into three regions:
- Supraglottis: Above vocal cords.
- Glottis: The vocal cords themselves. Hoarseness is an early sign here.
- Subglottis: Below vocal cords.
⚠️ Red Flag Symptoms: When to See a Doctor Immediately
Any of the following lasting more than 2-3 weeks requires evaluation by an Otolaryngologist (ENT):
- Persistent hoarseness or voice change
- A sore throat that does not resolve
- Pain or difficulty swallowing (dysphagia)
- A lump in the neck
- Ear pain on one side (otalgia)
- Unexplained weight loss and fatigue
:max_bytes(150000):strip_icc()/throat-cancer-symptoms-5093830_final-57e43814a47f4984b20a43a5719d3a63.jpg)
Visual overview of red-flag throat cancer symptoms
:max_bytes(150000):strip_icc()/is-it-a-lump-or-a-lymph-node-1191840-v1-5c869b3946e0fb00014319fb.png)
Neck lump – a common sign of lymph node involvement in throat cancer
Causes & Risk Factors: The HPV Revolution
The understanding of throat cancer causes has undergone a seismic shift with the recognition of HPV's role.
How HPV (especially HPV-16) causes oropharyngeal cancer – a major modern shift
| Risk Factor | Primary Cancer Link | Mechanism & Notes |
|---|---|---|
| Tobacco & Alcohol | Larynx, Hypopharynx, Oral Cavity | Synergistic effect. Heavy use of both multiplies risk up to 30x. The dominant cause of non-HPV cancers. |
| Human Papillomavirus (HPV-16) | Oropharynx (Tonsil, Base of Tongue) | Accounts for ~70% of oropharyngeal cancers in the U.S. Represents a distinct disease with better prognosis. |
| Betel Quid/Nut | Oral, Oropharyngeal | Common in Southeast Asia and South Asia. Contains areca nut and often tobacco. |
| Poor Nutrition | All Head & Neck Cancers | Diet low in fruits/vegetables. Antioxidant deficiency may play a role. |
| Genetic Syndromes | All (rare) | e.g., Fanconi Anemia, Dyskeratosis Congenita (extremely high risk). |
Diagnosis & Staging: The Roadmap
Accurate staging guides all treatment decisions.
Step 1: Clinical & Endoscopic Exam
Flexible Laryngoscopy: An in-office procedure using a thin camera to visualize the throat and voice box.
Step 2: The Biopsy & HPV/p16 Testing
Panendoscopy under anesthesia: Allows for thorough examination and biopsy. Critical Step: The biopsied tissue is tested for p16 protein, a surrogate marker for HPV. This result dramatically alters prognosis and treatment planning.
Step 3: Imaging
- CT Scan: Excellent for bone invasion and initial staging.
- MRI: Superior for visualizing soft tissue extent and perineural invasion.
- PET-CT: Gold standard for detecting metastatic disease and evaluating lymph nodes.
Staging (TNM + HPV Status)
The AJCC 8th Edition staging system has separate tables for HPV-positive (p16+) and HPV-negative oropharyngeal cancers, acknowledging their different behaviors.

HPV-specific staging in head & neck cancers – key differences from traditional staging
💡 The HPV Paradigm Shift
HPV-positive oropharyngeal cancer is now considered a distinct disease. Patients are often younger, non-smokers, and have a significantly better response to treatment. 5-year survival rates for advanced HPV+ cancer can be 80-90%, compared to 40-60% for similar-stage HPV- cancer. This has led to active research into "de-escalation" trials to reduce treatment intensity and side effects for HPV+ patients.
Modern Treatment Modalities
Treatment is decided by a multidisciplinary tumor board (surgeon, medical oncologist, radiation oncologist).
For Early-Stage (I/II)
- Single Modality Therapy: Either surgery or radiation alone.
- Minimally Invasive Surgery: Transoral Robotic Surgery (TORS) or Laser Microsurgery offer excellent cure rates with reduced morbidity.
Transoral Robotic Surgery (TORS) – minimally invasive approach for throat tumors (Mayo Clinic)
For Locally Advanced (III/IV)
- HPV-Negative / High-Risk: Standard is chemoradiation (often cisplatin + radiotherapy) or surgery followed by adjuvant (chemo)radiation based on pathology.
- HPV-Positive Oropharynx: Multiple pathways: de-escalation trials, standard chemoradiation.
- Immunotherapy: Drugs like Pembrolizumab and Nivolumab for recurrent/metastatic disease.
Prognosis & Survival: A Tale of Two Diseases
| Cancer Type / Factor | 5-Year Survival Range | Influencing Factors |
|---|---|---|
| HPV+ Oropharyngeal | 80 - 90%+ | Non-smoker, lower T-stage, lower nodal burden. |
| HPV- Oropharyngeal / Laryngeal | 40 - 70% | Heavily dependent on stage, continued tobacco use drastically worsens outcomes. |
| Early-Stage Glottic (Vocal Cord) | > 90% | Excellent with radiation or laser surgery; hoarseness enables early detection. |
| Advanced Hypopharyngeal | ~30 - 50% | Often presents late with subtle symptoms; historically poorer prognosis. |
Prevention & The Future
- HPV Vaccination (Gardasil 9): The most powerful preventive tool. Recommended for both males and females ages 9-45. This is a cancer-preventing vaccine.
- Tobacco Cessation & Alcohol Moderation: The most actionable personal steps to reduce non-HPV throat cancer risk.
- Screening & Awareness: No universal screening test exists. Public and clinician awareness of "red flag" symptoms is key to early diagnosis.
- Research Frontiers: De-escalation trials, immunotherapy combinations, and advanced imaging for better targeting.
Visit OncologyInsightsHub for the latest research summaries, treatment guides, and patient resources.



Comments
Post a Comment